Steff Noble, Pro Prep Head Coach, WNBF Pro

Menopause is a natural biological process that marks the end of a woman’s reproductive years. However, for many women, this transition is accompanied by a range of uncomfortable symptoms, including hot flashes, night sweats, mood swings, and vaginal dryness. In the past, Hormone Replacement Therapy (HRT) was often the go-to treatment for managing these symptoms. However, over the years, HRT has been the subject of controversy and mixed opinions. It’s time to reframe our understanding of HRT and explore its potential benefits for women’s health.
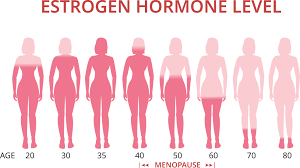
Traditionally, HRT has been primarily associated with alleviating menopausal symptoms. It involves the administration of estrogen and progesterone (in the case of women with a uterus) or estrogen alone (in women who have undergone a hysterectomy) to supplement the declining hormone levels during menopause. While HRT is undoubtedly effective in reducing hot flashes, night sweats, and vaginal dryness, its benefits extend far beyond symptom relief.
One of the key aspects of reframing HRT is recognising its role in preventing and managing long-term health issues. Hormone decline during menopause is linked to an increased risk of osteoporosis, cardiovascular disease, and cognitive decline. By restoring hormone levels through HRT, women can potentially reduce these risks and improve their overall health outcomes.
Studies have shown that HRT can help maintain bone density and reduce the risk of fractures associated with osteoporosis. Estrogen, in particular, plays a crucial role in bone health by promoting the activity of bone-building cells. By providing a steady supply of estrogen through HRT, women can strengthen their bones and mitigate the effects of age-related bone loss.

Furthermore, cardiovascular disease is a significant concern for postmenopausal women. Estrogen has been found to have a protective effect on the cardiovascular system, helping to maintain healthy blood vessels and reduce the risk of heart disease. While the Women’s Health Initiative study raised concerns about the cardiovascular risks associated with certain types of HRT, subsequent research has shown that the risks are dependent on factors such as the timing of treatment initiation and the type of hormones used. Individualised approaches to HRT, taking into account a woman’s age, health history, and personal risk factors, can help maximise the benefits while minimising potential risks.
Cognitive decline and dementia are also common concerns for women as they age. Estrogen has been shown to have neuroprotective effects, and some studies suggest that HRT may help improve cognitive function and reduce the risk of dementia. However, more research is needed to better understand the long-term effects of HRT on brain health.
Reframing HRT also involves promoting a more personalised and holistic approach to menopausal health. Every woman experiences menopause differently, with varying degrees of symptoms and underlying health conditions. By tailoring HRT to each individual’s needs, taking into account their specific symptoms, medical history, and preferences, healthcare providers can optimise treatment outcomes and address the unique challenges faced by each woman.
It is important to acknowledge that HRT is not suitable for everyone. Women with a history of breast or endometrial cancer, blood clots, or liver disease may be advised against HRT. Additionally, individual factors such as age, lifestyle choices, and personal preferences should be considered when deciding on the appropriateness of HRT.
In conclusion, reframing HRT for women involves recognising its potential beyond symptom relief. It offers significant benefits in terms of long-term health outcomes, including the prevention and management of osteoporosis, cardiovascular disease, and cognitive decline. By adopting a personalised and holistic approach to menopausal health, HRT can be optimised to suit each woman’s unique
